Introduction to Bone Grafting
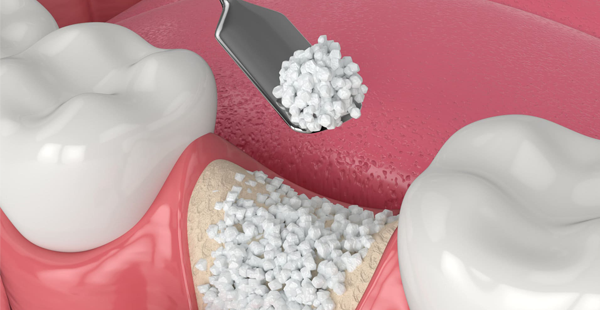
Bone grafting is a surgical procedure that involves the transfer of bone tissue to repair or regenerate damaged bones. This technique plays a crucial role in various medical and dental procedures, aiding in the restoration of normal bone structure and function. The primary purpose of bone grafting is to promote healing in areas where bone has been lost due to injury, disease, or other reasons, thus enhancing the body’s natural ability to regenerate bone.
In dental procedures, bone grafting is often necessary to create a stable foundation for dental implants. When a patient has experienced bone loss in the jaw, which can occur due to periodontal disease, tooth loss, or trauma, a dentist may recommend a bone graft. This procedure not only facilitates the successful placement of implants but also enables patients to achieve better overall oral health. The integration of grafted bone into existing bone tissue can significantly improve healing times and lead to favorable long-term outcomes.
There are several key terms and concepts associated with bone grafting that are essential to understand. Autografts, allografts, and xenografts are the three main types of graft materials used. An autograft involves harvesting bone from the patient’s own body, while an allograft uses bone from a donor, and a xenograft utilizes bone from another species. These different grafting materials each have unique properties and advantages in dental and medical applications.
Understanding bone grafting is vital for both practitioners and patients, as it underscores the importance of this procedure in enhancing dental health and restoring function. As the discussion progresses, various materials used in bone grafting will be explored, providing insights into their specific applications and effectiveness in promoting bone regeneration.
Types of Bone Grafting Materials
Bone grafting is a critical component of various dental procedures, particularly when it comes to dental implants and reconstructive surgeries. In the Philippines, several types of bone grafting materials are employed, each offering unique benefits and limitations. Understanding these materials can aid patients in making informed decisions regarding their dental health.
Autografts are considered the gold standard in bone grafting. These grafts are harvested from the patient’s own body, commonly from areas such as the hip or the mandible. The primary advantage of autografts is that they contain live cells, reducing the risk of rejection and promoting faster integration with the surrounding bone. However, the process involves an additional surgical site, which may increase recovery time and postoperative discomfort.
Allografts, on the other hand, are derived from human donors and processed to eliminate any live cells. These materials are readily available and can significantly shorten surgical time since they do not require an additional harvest site. Their effectiveness is well-documented; however, there is a slight risk of disease transmission, albeit extremely rare due to rigorous screening processes.
Xenografts are sourced from animal bones, typically bovine. These grafts undergo extensive sterilization to ensure safety. Xenografts serve as a scaffold for new bone growth, making them a viable option for patients who may not have sufficient bone density. While they are generally well tolerated, they can result in a slower healing process compared to autografts and allografts.
Lastly, synthetic bone grafts are made from biocompatible materials such as hydroxyapatite or tricalcium phosphate. These grafts do not involve any biological components, thus eliminating the risk of disease transmission. They can be molded to fit the required surgical site and encourage bone regeneration. However, they may not integrate as seamlessly as biological grafts.
Each graft type plays a pivotal role in various clinical scenarios within dental practices in the Philippines, allowing dentists to tailor treatments to the specific needs of their patients.
Autografts: The Gold Standard
Bone grafting has become an essential procedure in dentistry, particularly when restoring oral structures or repairing damaged bone. Among the various materials employed for this purpose, autografts are frequently regarded as the gold standard. An autograft refers to bone harvested from the patient’s own body, typically from areas such as the hip or the lower leg. This intrinsic relationship between patient and graft offers unique advantages that other graft types may not provide.
The biocompatibility of autografts is a primary reason they are so highly valued. Since the bone used is the patient’s own, there is a reduced risk of rejection as the body recognizes the grafted tissue as familiar. This leads to a more successful integration within the surrounding bone, showcasing a considerable potential for complete healing. From a dental perspective, this is vital for successful outcomes, especially in situations requiring significant reconstruction, such as dental implants following tooth loss.
However, the harvesting process of autografts is not without its considerations. Surgical extraction typically requires an additional incision, which introduces a recovery period for the patient apart from the graft site. This dual recovery can lead to heightened discomfort and, in some instances, complications such as infection or prolonged healing times. Furthermore, while autografts generally lead to effective results, the individual’s overall health and adherence to post-surgical care substantially influence recovery outcomes.
In conclusion, while autografts remain the gold standard in bone grafting due to their biocompatibility and integration potential, the implications of their use—including recovery times and potential complications—must be thoroughly discussed between the patient and their dentist. Balancing these factors is key to determining the most effective grafting strategy tailored to each individual’s needs.
Allografts: From Donors to Patients
Allografts represent a crucial innovation in dentistry and orthopedics, serving as viable solutions in bone grafting procedures. These grafts are sourced from deceased donors, providing a scaffold for the regeneration of bone tissue in patients requiring dental implants or reconstructive surgeries. The use of allografts has garnered increasing attention in the Philippines due to their effectiveness and the stringent regulations put in place for their acquisition.
The process of obtaining allografts involves meticulous screening and testing to ensure the safety and compatibility of the donor tissue. Regulatory bodies in the Philippines, such as the Food and Drug Administration (FDA), impose rigorous standards to minimize the risk of disease transmission. Donor bones undergo comprehensive evaluations, including infectious disease testing and compatibility assessments, to ensure they meet the highest safety standards. This thorough process not only protects patients but also enhances the reliability of allografts in dental applications.
The benefits of utilizing allografts in dental procedures are significant. One of the primary advantages is the reduction in surgical time compared to autografts, where the patient’s own bone is harvested. By using allografts, dental professionals can perform procedures more efficiently, leading to shorter recovery times for patients. Additionally, allografts eliminate the need for a second surgical site, thereby reducing overall morbidity and postoperative complications.
Despite their benefits, it is essential to acknowledge potential risks associated with allografts. These can include the possibility of immune rejection or, in rare cases, the potential transmission of infectious diseases. However, when sourced from reputable tissue banks that adhere to stringent guidelines, these risks are significantly mitigated. With a growing number of success stories in dental practices across the Philippines, allografts continue to establish themselves as a trusted material for bone regeneration, providing patients with effective treatment options and improved outcomes.
Xenografts: An Overview
Xenografts, which are bone graft materials derived from animals, have gained significant attention in the field of dental and orthopedic procedures. These grafts are primarily sourced from larger animals, such as cows (bovine) or pigs (porcine), due to the compatibility of their bone structure with human anatomy. The process of utilizing xenografts begins with the careful selection of donor animals, which are screened for diseases to ensure the safety of the graft material. Once selected, the bone is harvested and treated through a series of sterilization processes that typically include demineralization and dehydration. These processes help eliminate potential pathogens and enhance the biocompatibility of the graft, making it a safer option for human use.
Applications in Clinical Scenarios
In dental practices, xenografts are often employed in procedures that involve bone regeneration, particularly in cases of tooth loss or jawbone resorption. Dentists may recommend xenografts to augment the bone prior to dental implant placement, ensuring a stable foundation for the implants. Additionally, xenografts can serve as a filler material to repair bone defects due to trauma or disease. The adaptability of xenografts makes them a versatile choice for various applications, ranging from dental enhancement to complex surgical corrections.
Acceptance and Challenges
Within the Philippine healthcare system, the acceptance of xenografts varies among practitioners and patients. While many dentists recognize the efficacy and safety of xenografts, some patients express concerns regarding the origin of animal-derived materials. The cultural context may influence perceptions, prompting dentists to provide thorough education on the treatment processes and associated benefits. Moreover, the availability and cost of xenograft materials may pose challenges in rural areas where access to advanced dental supplies is limited. It is essential for the dental community to address these factors and promote understanding of xenografts to enhance their adoption in various clinical settings, ultimately improving patient outcomes and satisfaction.
Synthetic Bone Grafts: An Innovative Approach
Synthetic bone grafts are becoming increasingly prevalent in dental procedures, offering an innovative alternative to traditional grafting materials. These advanced materials are engineered to mimic the properties of natural bone, enhancing the success of dental implants and other restorative procedures. In the Philippines, the development and utilization of synthetic bone graft materials, including various biopolymers, have gained significant traction, reflecting a broader trend in dental advancements.
One of the primary advantages of synthetic bone grafts is their customization potential. These materials can be tailored to meet the specific needs of each patient, considering factors such as the density, shape, and structural requirements of the graft site. This customization is particularly beneficial in complex dental procedures where the unique anatomy of an individual’s mouth plays a crucial role in achieving optimal outcomes.
Moreover, synthetic grafts minimize the risk of disease transmission associated with human donor tissues. In traditional dental practices, the use of allografts often raises concerns regarding infections and immunological reactions. Synthetic options eliminate these risks, providing a safer choice for patients undergoing grafting procedures. The biocompatibility of these materials is also noteworthy. Many synthetic grafts facilitate new bone formation while integrating seamlessly with the surrounding tissue, ensuring higher success rates in dental applications.
Being at the forefront of dental innovations, the Philippines has seen a rise in research and development concerning synthetic bone materials. Local dental clinics and research institutions are investing in the study and application of these materials, leading to enhanced techniques that improve patient outcomes. As technology advances, the future of synthetic bone grafting in dentistry looks promising, with ongoing efforts to further refine these materials and expand their usage in various dental procedures.
Comparative Efficacy of Bone Grafting Materials
When considering the various bone grafting materials available, it is crucial for dental professionals and surgeons to understand their comparative efficacy. Each type of graft material showcases distinct characteristics that can impact integration rates and overall patient outcomes. The primary categories of bone grafting materials include autografts, allografts, xenografts, and alloplasts. Each of these options offers unique advantages and limitations in a clinical setting.
Autografts, derived from the patient’s own bone, tend to exhibit the highest integration rates due to their biocompatibility and the presence of live cells. According to studies, the success rate of autografts in periodontal and dental implant procedures is remarkable. However, harvesting these grafts can lead to increased surgical trauma and longer recovery times, which necessitates careful consideration by dentists when planning interventions.
On the other hand, allografts, sourced from human donors, provide a viable option that reduces the need for additional surgical sites. These materials have shown reasonable integration rates; however, the variability in cellular properties can affect the consistency of outcomes across different patients. In scenarios where autografts are not feasible, allografts often serve as a reliable alternative that is widely utilized in dental practices throughout the Philippines.
Xenografts, originating from animal sources, and alloplasts, synthetic materials, are notable for their ease of use and availability. While xenografts have demonstrated decent integration rates, they are typically less favored compared to autografts and allografts due to concerns regarding immunogenicity and long-term outcomes. Alloplasts, although convenient, may not integrate as effectively, leading to varying success rates in dental restorations.
In assessing the most effective bone grafting materials, dentists are encouraged to consider the unique circumstances of each patient. The choice of material not only affects the integration and healing process but also influences long-term results, making it essential for practitioners in the Philippines to stay updated on innovative grafting solutions.
Future Trends in Bone Grafting
Advancements in bone grafting technologies are set to revolutionize the practice of dentistry and medicine, particularly in the Philippines. As the demand for effective dental procedures rises, emerging trends indicate a move towards innovative materials and techniques that promise improved outcomes for patients. Among these developments, bioactive graft materials are gaining traction. These materials are designed to interact positively with the body, promoting faster healing and integration with existing bone tissue. The use of bioactive grafts could enhance the success of dental implants, ultimately benefiting dental practitioners and their patients alike.
Moreover, stem cell therapy is emerging as a game-changer in the realm of bone regeneration. By utilizing stem cells, dentists and medical professionals can potentially stimulate the body’s natural ability to heal and regenerate bone. This method not only supports the integration of dental implants but also minimizes recovery time. The incorporation of stem cell therapy into bone grafting procedures may soon become commonplace in the Philippines, allowing patients to experience more effective and less invasive treatment options.
The advent of 3D printing technology is another notable trend shaping the future of bone grafting. This innovative approach allows for the precise creation of custom bone graft scaffolds, tailored to each patient’s specific anatomical needs. Such technology enables dentists to design grafts that promote optimal integration and support healing processes. As 3D printing becomes more accessible in dental practices, it is expected to streamline procedures, reduce costs, and enhance patient outcomes significantly.
The combined impact of these innovations is poised to redefine the standards of care within dentistry in the Philippines. With ongoing research and development, the future of bone grafting promises to bring forth safer, more efficient, and patient-centered solutions. As dentists and medical professionals embrace these advancements, the potential for improved healing and enhanced quality of life for patients becomes increasingly attainable.
Conclusion: Selecting the Right Material
In reviewing the various bone grafting materials available in the Philippines, it becomes evident that the choice of the appropriate graft is pivotal for successful outcomes. The effectiveness of any dental procedure, particularly in the context of bone grafting, relies heavily on understanding the unique needs of each patient, the clinical scenario being addressed, and the specific resources available within local healthcare settings. The materials discussed, ranging from autogenous grafts to synthetic options, each hold distinct advantages and potential limitations that must be balanced carefully.
When selecting a grafting material, it is essential for dentists to perform a thorough assessment of the patient’s medical history and their specific orthopedic or dental needs. Factors such as the site of the graft, the desired healing time, and the patient’s overall health should guide the decision-making process. Furthermore, staying informed about the latest advancements in bone grafting technologies and materials can significantly enhance clinical practice, leading to improved patient outcomes.
Given the evolving landscape of dental medicine, continual research and adaptation are necessary. Dental professionals must engage with emerging studies and innovations to ensure that their practices reflect the best possible standards. Collaboration with colleagues and participation in specialized training can provide valuable insights into novel procedures and materials that may benefit patients in the Philippines.
In conclusion, selecting the right bone grafting material is a multifaceted decision that demands careful consideration and expertise. By prioritizing patient-centered approaches and remaining adaptable in the face of new research and technologies, dentists can significantly enhance the efficacy of their treatments, ultimately contributing to the advancement of dental care in the region.

Leave a Comment
Your email address will not be published. Required fields are marked *